By Elizabeth Heubeck
Recommend Tweet Email Print More
The fallout from the pandemic has run the gamut from an unstable economy to an uptick in social-emotional problems. Experts suggest the pandemic may also be responsible for a continued upward trajectory in sexually transmitted diseases among Connecticut’s youngest sexually active residents.
Conditions during the pandemic, including less access to sexual health care and more free time, have helped to exacerbate the trend among young people, say health care providers. “Most parents are working. Students are home alone. They are having friends over,” said Ceri Burke, a nurse practitioner at Danbury High School’s on-site health center. “There’s an increase in sexual activity among the kids I’m seeing.”
These factors, coupled with recent data trends, suggest a continued upward trajectory of sexually transmitted diseases (STDs) during the pandemic among adolescents, with Black teens being disproportionately affected.
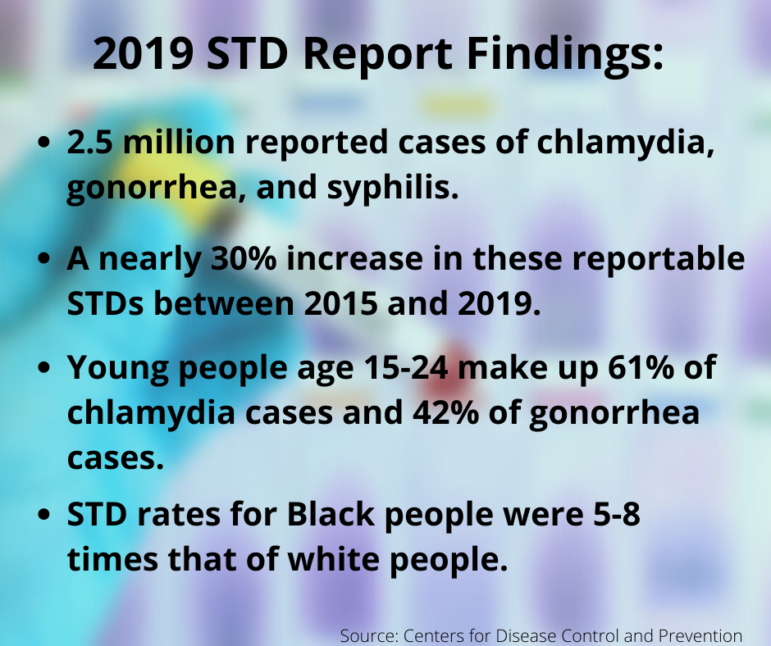
In 2019, national data from the Centers for Disease Control and Prevention (CDC) showed STDs had risen to their highest level for the sixth consecutive year, a statistic some blame in part on the Trump administration’s dismantling of accessible and affordable health care and associated educational resources and programming. Adolescents and young adults (ages 15-24) make up a disproportionate share of these numbers; adolescents of color are especially hard hit.
CDC data from 2018, for instance, showed the rate of reported chlamydia cases among Black females aged 15–19 years was 4.5 times higher than among their white female counterparts; for Black males in this age group, the rate was 9.1 higher than white males in the same age range. And in Connecticut, the chlamydia rate among women ages 15 to 24 was nearly 12 times higher among Blacks than among whites in 2014, according to data from the state Department of Public Health (DPH). Further, statistics point to similar differences along racial lines for other STDs.
Virtual Education Continued During The Pandemic
A program at Yale has sought to better understand and address these disparities. The Yale Center for Health & Learning Games is working to empower Black adolescent girls around dating and sexual experiences. Virtual focus groups with Black teen girls have been a big part of this endeavor.
“We really wanted to understand what it means to date as a Black teen girl,” said the center’s deputy director, research scientist Kimberly Hieftje.
The focus groups revealed barriers to healthy attitudes about sexuality common to this demographic: hypersexualism, colorism and other stereotypes. These challenges, coupled with a mistrust of health providers, impact Black teen girls’ attitudes and behaviors around sexual health, Hieftje said.Pandemic Fuels Continued Rise In STDs Among Youngest Sexually Active Adolescents

Kimberly Hieftje Yale Photo
To help combat these challenges, the center has devised a video game that uses role-playing and requires users to navigate situations like discussing condom use with their partners and getting tested for STDs. Ultimately, the purpose is to empower players to become adept at controlling their sexual health. The center’s researchers hope to make it available for use in schools and other public forums.
Elsewhere in Connecticut, virtual sex education efforts have continued during the pandemic. For example, Planned Parenthood of Southern New England offers a peer education program, STARS (Students Teaching About Responsible Sexuality), promoting healthy relationships through responsible choices. As part of the program, Planned Parenthood trains teens to respond to basic questions from their peers on sexuality-related topics and recognize when and how to make referrals to professional sources. During the pandemic, the peer ambassadors created videos on TikTok about STDs and the importance of getting tested for them—a service that, along with STD treatment, is among Planned Parenthood’s most utilized.
Access To Sexual Health Services Declined During Pandemic
Knowing about the importance of STD testing isn’t the same as having easy access to testing. Since March 2020, when schools in Connecticut closed their doors—some for several months—adolescents have had reduced access to convenient, confidential sexual health services that protect against and screen for sexually transmitted diseases.
In a typical year, school-based health centers (SBHCs) serve as the most convenient, accessible and confidential source of sexual health services for adolescents. According to the DPH, 20,216 students made 62,159 medical visits to school-based health centers in 2018-2019, an average of 3.1 visits per student.
SBHC health care providers routinely ask adolescent patients if they’re sexually active. When patients respond in the affirmative, they are urged to undergo confidential STD testing; a right afforded to all minors 12 years and older under Connecticut state law. Many SBHCs also provide testing services on site.
But during the pandemic, as schools operated remotely or in a hybrid capacity, even SBHCs that did not close saw far fewer students. Angela Matera, a nurse practitioner at Stratford High School’s SBHC, says she usually sees 14 kids a day, five days a week, 190 days a year for various medical needs. That changed during the pandemic.
“It was a lot more uncomfortable for these kids,” said Matera, who tracked students on a spreadsheet during the pandemic and attempted to contact those she deemed high risk.
Since March 2021, when students in Stratford returned to campus, Matera has seen “an enormous rise” in positive STD cases: nine cases of chlamydia, two cases of oral chlamydia and gonorrhea. “That’s a jump,” Matera said.Alyssa Bennet

Alyssa Bennet CCMC photo
Other health care providers also report having less contact with adolescent patients during the pandemic. Dr. Alyssa Bennett, head of adolescent medicine at Connecticut Children’s Medical Center, says many teens who might normally be tested for STDs were slipping through the cracks during the pandemic. “It’s very hard to test a patient for an STD if they’re not in your clinic,” she said.
Bennett says she inquires about sexual activity during the private, one-on-one portion of the visit with her adolescent patients, a practice recommended by the American Academy of Pediatrics. She then offers to perform STD testing. “I very rarely have teens decline testing once they know we can provide it confidentially,” Bennett said. But many adolescents are unaware of their legal right to confidential sexual health services. It’s just one of several gaps in adolescents’ sexual health awareness.
Bennett says that many adolescents don’t know you can be asymptomatic with an STD. “If you don’t ask a teen if they’re having sex, you’re not going to think about asking about [STD] testing,” Bennett said.
Support Our Work
The Conn. Health I-Team is dedicated to producing original, responsible, in-depth journalism on key issues of health and safety that affect our readers, and helping them make informed health care choices. As a nonprofit, we rely on donations to help fund our work.Donate Now