By Cara Rosner
By Cara Rosner
When the pandemic began, LaVita King of Bridgeport worried about how she would continue to see her behavioral health therapist and primary care physician at Southwest Community Health Center.
She lives close enough to walk to the federally qualified health center but didn’t feel comfortable leaving her home in those early days, let alone venturing into a medical office. But she’s been able to access care through phone and video chats.
“For me, it’s been such a lifesaver, such a blessing,” said King, 69. “Otherwise, I would not have been able to talk to my behavioral health therapist for this whole entire time. The fact that I could speak with her on the phone every week—and then we figured out a way that we could actually see each other on video—it’s just a blessing.”
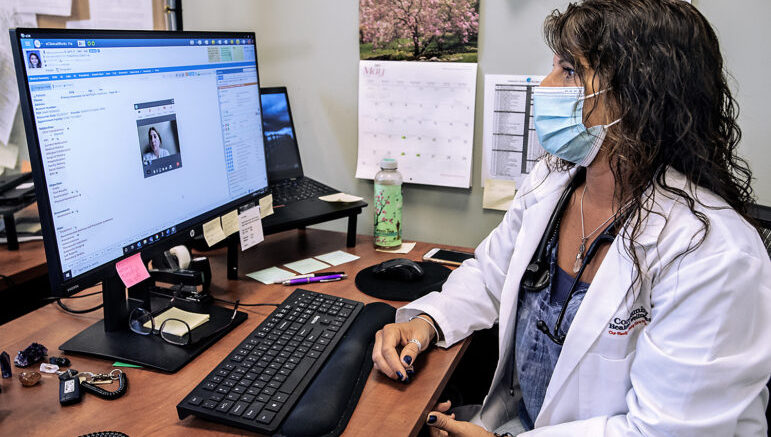
Darcy Cusano, an advanced practice registered nurse at the Community Health & Wellness Center in Torrington, meets with a telehealth patient.
Telehealth has helped connect patients to providers over the past year. It has been particularly crucial in keeping federally qualified health center (FQHC) patients, many of whom are people of color and on Medicaid, connected to medical care during the pandemic.
But while telehealth has brought some health care benefits and kept those already receiving services connected to their providers, national reports by Robert Wood Johnson Foundation and Health Affairs show that the technology has done little to reach new patients, and those with limited English proficiency had low rates of telehealth use.
FQHCs are community-based health care providers that receive federal funds to provide primary care services in underserved areas. They must meet a stringent set of requirements, including providing care on a sliding fee scale based on ability to pay and operating under a governing board that includes patients.
According to Ken Lalime, CEO of the Community Health Center Association of Connecticut, 62% of FQHC patients in Connecticut are on Medicaid, 10% are on Medicare and 15% are uninsured. Most, around 90%, have income that’s twice the federal poverty level, and more than half don’t speak English as their first language. There are 17 FQHCs in Connecticut.
FQHCs saw their number of patient visits plummet as soon as the COVID-19 pandemic hit, Lalime said. Providers wondered how they would reach their at-risk patients and get them the care they needed. Telehealth quickly emerged as the answer.

“Just because we built it doesn’t mean that folks will come. What most data are showing across the country is that [telehealth] made access more readily available for people who already had access.”
Tekisha Dwan Everette,
executive director of Health Equity Solutions
On March 10, 2020, Gov. Ned Lamont issued an executive order that, among other things, allowed Medicaid to cover telehealth visits. On May 10, 2021, he signed legislation into law that extends that provision for another two years.
“Telehealth meant everything for people getting access to care in the pandemic,” said Jill Zorn, senior policy officer at the Universal Health Care Foundation of Connecticut. “From a health care perspective, not being able to see your doctor was a real problem. Having [insurers, including Medicaid] pay for telehealth was huge. If there’s any good thing that came out of the pandemic, this is one of them.”
When COVID shutdowns began, FQHCs in the state saw patient visits drop by up to 80%. Once the state allowed telehealth, some centers conducted as much as 80% of their visits that way, and over the past year or so, about 50% of all FQHC visits have been telehealth visits, Lalime said. The number of telehealth visits is starting to drop now, he said, as patients feel more comfortable scheduling in-person visits.
‘A Game Changer,’ But Not For All
Via telehealth, King has continued her care plan, gotten referrals for any tests or scans she needs, and ensured her prescriptions stayed up to date.
“All of the things that I needed to have done because I have access to my providers through telemedicine, I’ve been able to have those things done,” she said.
Staff at Southwest Community Health Center in Bridgeport had long been interested in telehealth, but it was never feasible before because Medicaid wouldn’t cover the expense, said the center’s president and CEO, Mollie Melbourne.
“Telehealth was a game-changer for us. It really helped us retain that connection with our patients,” Melbourne said. She added that it was essential for patients receiving mental or behavioral health services and those with chronic illnesses.
“Technology was a challenge [early on] but the concept of telemedicine, they fell right into. The patients seem to love it, especially for behavioral health,” Melbourne said. “And once we got over the technological hurdles, the providers really enjoy it.”
Telehealth eliminates various barriers to care, including the need for transportation, said Joanne Borduas, CEO of Community Health & Wellness Center, which has locations in Torrington and Winsted.
“We have no public transportation at all” in the area, she said. “It’s a challenge as it is, without a pandemic, trying to keep our patients coming back and staying connected with them. The ability to stay connected to them is so critical to their health and wellness,” she said.
Without telehealth, Borduas said, “we probably would have seen an enormous increase in adverse outcomes. What that would have caused is just this cycle throughout the pandemic of [patients] having their needs met in the emergency room. We were very happy that we were able to use telehealth.”
Telephone telehealth, in particular, has been a lifeline for many, she said.
“Not all of our patients have the ability or the money to buy computers, so the ability to do video telemedicine was challenging,” she said. “The telephone-only component was really a lifeline for many of our patients; it became such a huge component.”

Ken Lalime
Telehealth has brought various benefits but also new challenges.
“There were definitely some growing pains,” Lalime said. “To get it rolling, it took patient education and system education. Connecticut responded fairly quickly to this, but it was not instantaneous. It took some time.”
The Community Health Center Association is studying the impact of telehealth and how well it worked during the pandemic, he said.
‘The Key To Equity?’ Not So Fast
While telehealth likely helped centers recoup the patients they had lost in the pandemic’s early days, early data show it hasn’t improved overall access to care, said Tekisha Dwan Everette, executive director of the advocacy group Health Equity Solutions.
“Just because we built it doesn’t mean that folks will come,” she said, noting many FQHC patients lack access to the broadband internet needed for video visits. “What most data are showing across the country is that [telehealth] made access more readily available for people who already had access.”
She’s encouraged by proposals to expand broadband access in the state, she said, but other questions remain. As centers consider telehealth’s role, they need to examine whether they are using it to be truly equitable. They need to assess whether it’s accessible to patients across various races and age demographics, for instance, and whether primary care is fully embracing it, she said.
“Everybody thinks this is the key to equity—which it can be—but when they start to look at their data, they realize it isn’t,” she said. “I think we can do it right; I don’t necessarily think we did it right.”

“From a health care perspective, not being able to see your doctor was a real problem. Having [insurers, including Medicaid] pay for telehealth was huge. If there’s any good thing that came out of the pandemic, this is one of them.”
Jill Zorn, senior policy officer at the Universal Health Care Foundation of Connecticut.
FQHCs will be able to use telehealth for at least the next two years, but leaders hope it is here to stay.
“There are some things, we all know, that simply can’t be done over telemedicine,” Melbourne said. “But I see it as a critical tool. I hope it does not go away.”
Borduas said, “There will always be a place for telemedicine. We’re going to prepare to do this forever. That technology will be embedded in everything we do going forward.”
Telehealth will never fully replace in-person care, Lalime said, but “it’s part of the toolkit. Over the next couple of years, I think it’s going to evolve. It’s a very exciting time.”
Support Our Work
The Conn. Health I-Team is dedicated to producing original, responsible, in-depth journalism on key issues of health and safety that affect our readers, and helping them make informed health care choices. As a nonprofit, we rely on donations to help fund our work.Donate Now
Subscribe to our monthly newsletter!
Get news from the Connecticut Health Investigative Team in your inbox. Email
By submitting this form, you are consenting to receive marketing emails from: Connecticut Health Investigative Team, 346 Alden Avenue, New Haven, CT, 06515, US, http://www.c-hit.org. You can revoke your consent to receive emails at any time by using the SafeUnsubscribe® link, found at the bottom of every email. Emails are serviced by Constant Contact. http://www.google.com/recaptcha/api2/anchor?ar=1&k=6LfHrSkUAAAAAPnKk5cT6JuKlKPzbwyTYuO8–Vr&co=aHR0cDovL2MtaGl0Lm9yZzo4MA..&hl=en&v=CdDdhZfPbLLrfYLBdThNS0-Y&size=invisible&cb=j9jdrzczbie2

Related Stories
- Care Coordinators Cut Costs, Improve Health Outcomes, But Are Underused A few years ago, patient navigators at Project Access-New Haven set out to see if they could change the course of health care treatment for some Medicaid patients who frequently used emergency rooms. They contacted emergency departments at Yale New Haven Hospital and its Saint Raphael campus and enrolled 100 patients in their study in 2013. Those selected had visited emergency rooms four to 18 times in the past year for chest pain, abdominal pain or chronic migraines, among other ailments.