By Carol Leonetti Dannhauser
Recommend Tweet Email Print More

Sweating in his black jacket under a brilliant spring sun, Keith J. DuPerry, 40, waited in line on the New Haven Green. Destination: FEMA’s first-in-the-nation COVID-19 mass vaccination trailer, administered by Griffin Hospital of Derby.
Earlier that morning, DuPerry had taken a bus from the sober house where he lives to an addiction treatment center downtown. The buzz of activity on the Green—party tents and comfortable seating, trailers custom shrink-wrapped with photos of smiling, diverse, shot-giving caregivers and grateful patients—got him thinking.
He returned to the Green after lunch. “I was sitting on a bench, trying to figure out if I should get the vaccine. Somebody was nearby, listening to gospel music. I took that as a sign that this was meant to be. I thought, this is a new beginning.”
By day’s end, DuPerry was among about 625 people vaccinated at the Griffin-run clinic. Hundreds more received shots there the next day—all in the shadow of the state’s largest hospital, Yale New Haven, the monolith about six blocks west.
During the darkest days of the pandemic, Griffin Hospital stepped up to reach many of Connecticut’s most neglected communities. Even as the hospital was losing millions of dollars a month, Griffin agreed to test nursing home residents and employees on-site, and later to administer vaccines.
When prisoners and guards fell through the cracks of care, Griffin came to the state Department of Correction’s aid.
When the state Department of Public Health (DPH) struggled to bring vaccines to the most inaccessible—those with developmental needs and those struggling with addiction—Griffin seemingly overnight created and staffed a mobile health fleet 36-vehicles strong to do the job. All the while, tripling its ICU capacity and continuing to treat the sickest patients at its 160-bed hospital in Derby.
“They’ve been a really strong, important partner with the state throughout the pandemic,” said Dr. Deidre Gifford, acting DPH commissioner. Other health organizations came and receded during the pandemic, she said, but Griffin brought willingness, staff, “and, frankly, competency” to the state’s efforts. “They’ve been very good at this work.”
In many ways, COVID-19 may have sparked a new beginning for the hospital itself.
Sounding The Alarm
Griffin Hospital sits in the center of Derby, tucked in the elbow between the Housatonic and Naugatuck rivers. Used-car dealerships, grocery stores and fast-food outlets pepper the neighborhood nearby. About 13% of Derby’s 12,500 or so residents live in poverty, with an average per capita income in 2019 of $31,936, according to the U.S. Census.
At the turn of the 20th century, the lower Naugatuck River Valley was a bustling brass manufacturing center, and community leaders in Derby, the state’s smallest city at just under 5.5 square miles, started fundraising to build The Derby Hospital.
A local industrialist, George Griffin, who’d made his fortune turning animal horns into buttons, bequeathed some riches to the effort, and Griffin Hospital was born. The first patient at the 24-bed hospital was a brass worker from Ansonia.
Griffin Hospital served the Valley community during its most challenging moments: two trolley accidents; the flu pandemic of 1918; and one of the worst disasters in Connecticut history, the flood of 1955, in which 87 people died. During that time, many of the state’s hospitals were gobbled up by big health care systems.
Not Griffin, though. Of the state’s 28 acute-care hospitals, according to the Connecticut Office of Health Strategy, Griffin is one of seven that remain independent. The pandemic threatened them all.
In January 2020, two months before COVID-19 reached Connecticut, Griffin’s chief medical officer, Dr. Frederick Browne, didn’t like what he was seeing.
Browne, an epidemiologist and expert in pandemic flu, predicted to Patrick Charmel, Griffin’s president and CEO, that the virus could reach Connecticut in weeks. Charmel, whom staff members say is a hands-on leader unusual in the upper echelons of health care administration, established a command center on-site, and his team met daily.
Without the deep pockets of bigger hospitals, but with a nimbleness that many lack, the Griffin crew got creative. Before the first case hit Derby, local businesses donated ventilators, and Griffin refurbished CPAP machines to double as back-ups.
Griffin retrofitted a decommissioned pod of 20 beds and turned it into a negative pressure unit, so that clean air could enter and circulate—with infected air filtered and transported outside—without contaminating the rest of the hospital.
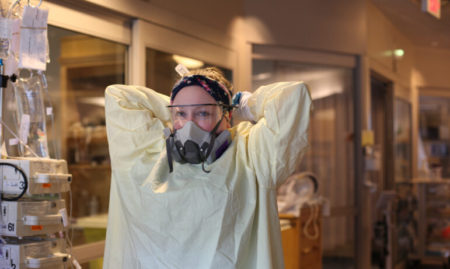
The operations director sourced enough personal protective equipment outside of normal hospital channels to last through the pandemic. The engineering team constructed a box out of plexiglass to help turn critically ill patients to a prone position.
“Because we started this before anyone else, we were able to locate everything we needed for our ICU before we had one case,” Browne said.
Dr. Marya Chaisson, a pulmonary care expert who directs the ICU at Griffin, said, “Every time I went down to the command center, [Charmel] was down there, dealing with every problem. I remember Pat working there, waiting for the plexiglass to dry. He was not afraid to get his hands dirty. I’d never seen anything like it. It was so inspiring. At so many other hospitals, administrators were just gone, working from home, nowhere to be found.”
The rest of Griffin grew eerily quiet.
“People weren’t seeking all of the outpatient services like they had,” said Jim Moylan, a former CFO at Griffin, Bristol and Waterbury hospitals. “With a small community hospital, a lot of the profit they get comes from their outpatient services, things like mammography and lab tests, or from surgeries that are elective, like a knee replacement.”
Trips to the emergency room, which had exceeded 32,000 in 2019, as well as imaging procedures, clinical visits and more added to Griffin Health’s $223 million operating revenue in 2019, according to the Connecticut Office of Health Strategy. The Connecticut Hospital Association warned that hospitals could lose as much as $400 million a month in revenue. A report from the American Hospital Association predicted a “dire and unstainable outlook.”

Suddenly, said Browne, “We got slammed! The ED was full of COVID patients. All of a sudden, 40% of our patients are COVID. In that first wave, there were a lot of very sick people. Once we were in the thick of things, you had to assume everybody had COVID-19. But we were ready for it. The entire ICU unit we converted to a COVID unit.”
Browne’s job was to keep the staff safe. Chaisson’s was to care for the most critical patients. Charmel’s was to keep the hospital afloat.
Without its money-makers, Griffin expected to lose $6 million a month. The hospital redeployed 70 staff members to tackle the COVID-19 surge—and furloughed 99 others. Everyone, from management on down, took a pay cut of up to 20%. The pandemic threatened to take down the entire community around and including the hospital.
Game-Changer
Before large-scale testing sites existed in Connecticut, Griffin constructed a drive-through site in a parking lot. They staffed it seven days a week and told test-takers to quarantine until results came in. While other hospitals suspended procedures indefinitely, Griffin’s testing enabled procedures to resume faster. “That became a game-changer for us,” Browne said.

Inside the hospital, patients filled the ICU from nearby nursing homes. To stem the spread, Charmel brought testing to the nursing homes despite losing money on each test. In June 2020, before Gov. Ned Lamont ordered all nursing home staff and residents in Connecticut to undergo weekly COVID-19 testing, DPH officials called Charmel.
“They said, ‘We heard you’re doing lab testing,’” Charmel recalled. “I said we have 10 [nursing homes]. They said, ‘Can you do a few more?’ Within a month, we were doing 124 nursing homes [out of the state’s 209]—every resident and every staff member weekly. We started drive-through in five locations. At the height of testing, we were doing about 35,000 people a week.”
All that testing required equipment, staffing and supplies. When the sterile Viral Transport Media used to transport all those swab samples couldn’t be sourced, Charmel had Griffin’s internal lab develop its own. When the wait for lab results lagged to a week or longer, Charmel bought processing equipment and expanded Griffin’s in-house test team. The hospital was hiring again.
DPH Acting Commissioner Gifford said, “They helped us with state employee testing, Department of Corrections, Department of Developmental Services, Department of Addiction. They did over 15,000 tests for state employees.”
By August, a million Connecticut residents had been tested. The same month, the hospital received $8.7 million in federal relief from the CARES Act high impact funding with the help of U.S. Rep. Rosa DeLauro, D-3rd, on top of another $4.6 million secured earlier from the CARES Act.
By December, vaccines became available. Charmel and crew transformed a vacant building in Shelton into a mass vaccination center. “I was saying ‘We can do this, and we can do that.’ They must have been saying ‘Are you crazy? It’s New Year’s Eve!’” Charmel said. He was leading the way, though, working alongside staff as 2020 ended. Griffin vaccinated more than 1,000 Connecticut residents there on opening day in January.
Community Reach

By spring, Griffin’s fleet of vaccine vans, staffed with 147 new hires, zigged and zagged across Connecticut, administering up to 100 vaccines each per day in underserved communities. They set up shop in Walmart parking lots, high school gymnasiums, recreation centers, church halls. State insurance marketplace Access Health had canvassed the neighborhoods, searching for people who couldn’t otherwise access vaccines, and the DPH sent Griffin’s vans in response.
“We have a lot of people living in substandard housing in our state. During COVID-19, who do you think died? People dying were disproportionately in the Black and brown community. That’s why we have this mobile program,” Charmel said.
It’s a curious dichotomy, working to improve community health while running a hospital. The healthier a community, the fewer clinical services members of that community will need, and the less revenue the hospital generates. But community care is at the center of Griffin’s mission.
Charmel, who graduated from the Yale School of Public Health and started working at Griffin as a college intern more than 40 years ago, believes that prevention efforts in compromised communities should be part of a hospital’s mandate. Griffin runs the state’s only preventive medicine training program, a four-year residency for doctors that combines internal medicine with preventive medicine.
During the pandemic, the community inside the hospital seemed to grow stronger. In hospital interviews and phone conversations, at testing sites and vaccination pop-ups, many Griffin employees repeated a version of something they’d heard Charmel say during lock-down: Twenty years from now, people are going to ask what you did during COVID. Were you home on the sidelines? Or were you doing something about it?
On a chilly day in late spring, as Connecticut’s COVID-19 vaccine rates inched up and infection rates fell, Griffin’s vaccine fleet set up shop at Rockwell Park Pavilion in Bristol, 2 miles from Bristol Hospital. Skateboarders zipped around the park. National Guardsmen worked the door. Pop music wafted inside. Three vaccination stations operated by new Griffin hires stood ready, waiting for walk-ins.
Jacob Martin, 19, wandered in, toting his skateboard. He sought the shot not so much for himself, he said, but so he could spend time with his grandfather, who had kept his distance during the pandemic.
“I thought about having the summer again. About spending time with my grandfather and going to shows.” He offered his left arm, as he planned to get a tattoo on his right later in the day. Dominique Mosley, a vaccinator new to Griffin, reminded him to “stay hydrated and get a lot of rest.” Eyeing the skateboard, she told him not to overdo things.
“I’m stoked at how easy this was,” Martin said as he rested in the cool pavilion before heading back out.
Behind him, vaccinator and van driver Lauri Jepsen, a retired Fairfield firefighter, readied her station for the next patient. The work so far had not been easy. She’d crisscrossed the state from morning until night, but she relished the work after so much time in quarantine. Her comment sounded familiar: “I’m happy to help turn this around and maybe be part of the solution.”

Scenes Of Survival
Today at Griffin, the negative pressure pod has been dismantled, the tubing scattered like giant Slinkys around the hospital roof. The command center is a memory now. But Griffin’s presence extends beyond the building and beyond the Valley.
“Griffin has been doing incredible things all over the whole state during COVID,” DeLauro said. “Now, everybody knows who they are.”
Money continues to trickle in. In May 2021, FEMA reimbursed the hospital $2.078 million for the pod and the testing tent. Earlier in the year, Lamont gave Griffin $1.758 million out of $40 million granted to hospitals statewide.
At the hospital, elective procedures are returning. Chaisson, who spent many nights attempting to sleep on the green chair in her office only to chase away the “horrifying, frightening” events of the day, sees her sleep apnea patients again.
In the cafeteria, employees line up at the wood-burning stove for whole-grain pizza. Visitors are ducking into the meditation center again. Health care workers, most of whom were rehired after the furlough, congregate outside in the lush green courtyards. In a year of so much death and loss, the perennials have returned, and so have many of the people.
So far, anyway, Griffin has survived.
Support Our Work
The Conn. Health I-Team is dedicated to producing original, responsible, in-depth journalism on key issues of health and safety that affect our readers, and helping them make informed health care choices. As a nonprofit, we rely on donations to help fund our work. Donate Now

Related Stories
- Street Medicine: Helping The Homeless Where They Live Homeless people tend to have trust issues, but when Phil Costello approaches they typically greet him like family. That’s because Costello, the clinical director for homeless care at Cornell Scott-Hill Health Center in New Haven, puts effort into building relationships and trust so he can get people the medical care they need.
More From C-HIT
- ctwatchdog.com Americans Can Purchase Drugs From Canada
- Disparities Yale Study Links Housing Instability And Risky Sexual Behaviors
- Environmental Health Medical Providers Are Taking Nature Therapy Seriously
- Fines & Sanctions UPDATED: Coronavirus In Connecticut
- Generation Health Failed Flavored-Tobacco Ban May Produce A Silver Lining For Teen Prevention Efforts


